
Statins regulate CD147 levels and induce changes in the CD147 structure, function, and expression via blocking N-glycosylation and isoprenylation of the proteins. Another therapeutic candidate for decreasing the actions of the S protein on the CD147 receptor is statins. Other humanized anti-CD147 antibodies such as metuximab and metuzamb have been developed and found to have a favorable safety profile however, their effects in COVID-19 are less well characterized. The condition and recovery rate of patients with COVID-19 pneumonia was improved with meplazumab treatment while maintaining a safety profile. Meplazumab inhibits the interaction between CD147 and the S protein in a dose-dependent manner. A humanized anti-CD147 antibody that has been examined in SARS-CoV-2 pneumonia is meplazumab. The finding that CD147 receptor can mediate non-infective COVID-19 microvascular disease has therapeutic implications. The identity of the proinflammatory actions of the S protein on pericytes remains to be determined.
Interestingly, the effects of the S protein to secrete proinflammatory cytokines to induce endothelial cell death occurred by a mechanism independent of the CD147 receptor. used a CD147 blocking antibody or mRNA silencing approach to determine that the S protein activation of cardiac pericyte CD147 receptors resulted in ERK1/2 signaling to exert detrimental effects. Activation of CD147 mediates macrophage inflammation, induction of MMP-9 expression, and cytokine expression in endothelial cells.
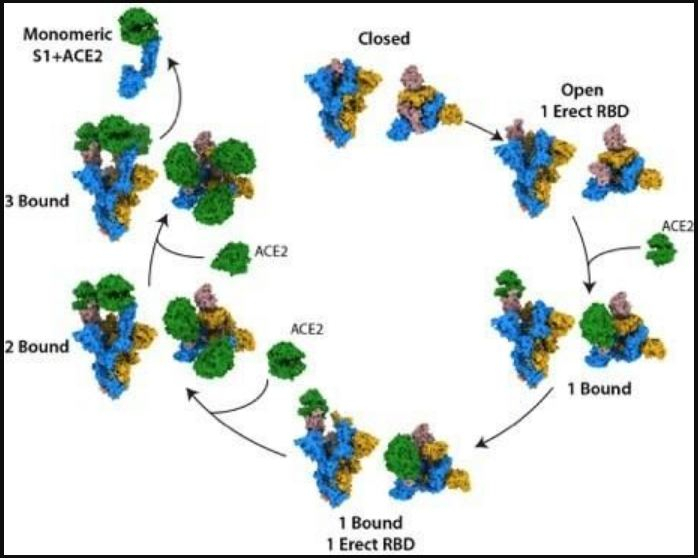
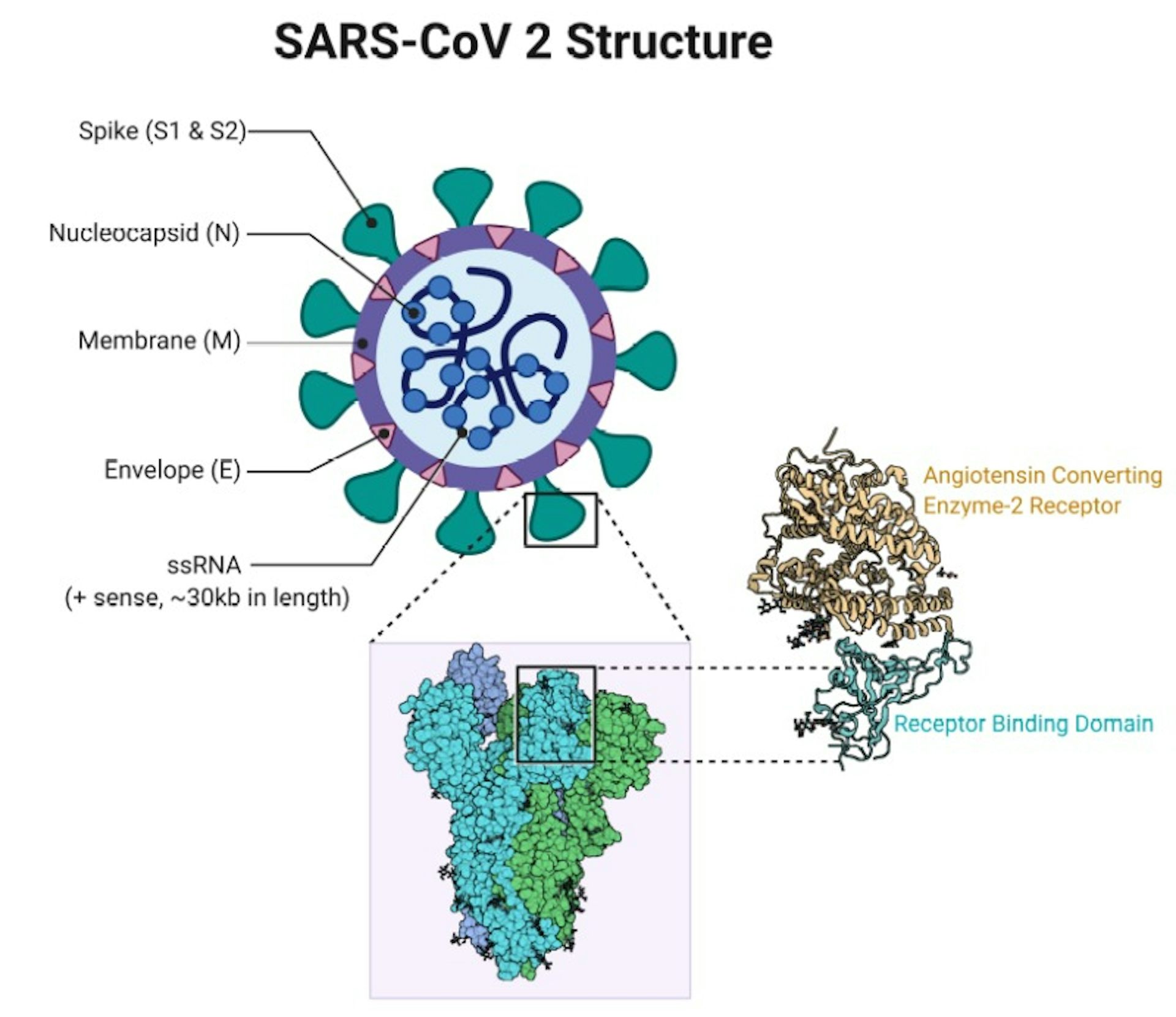
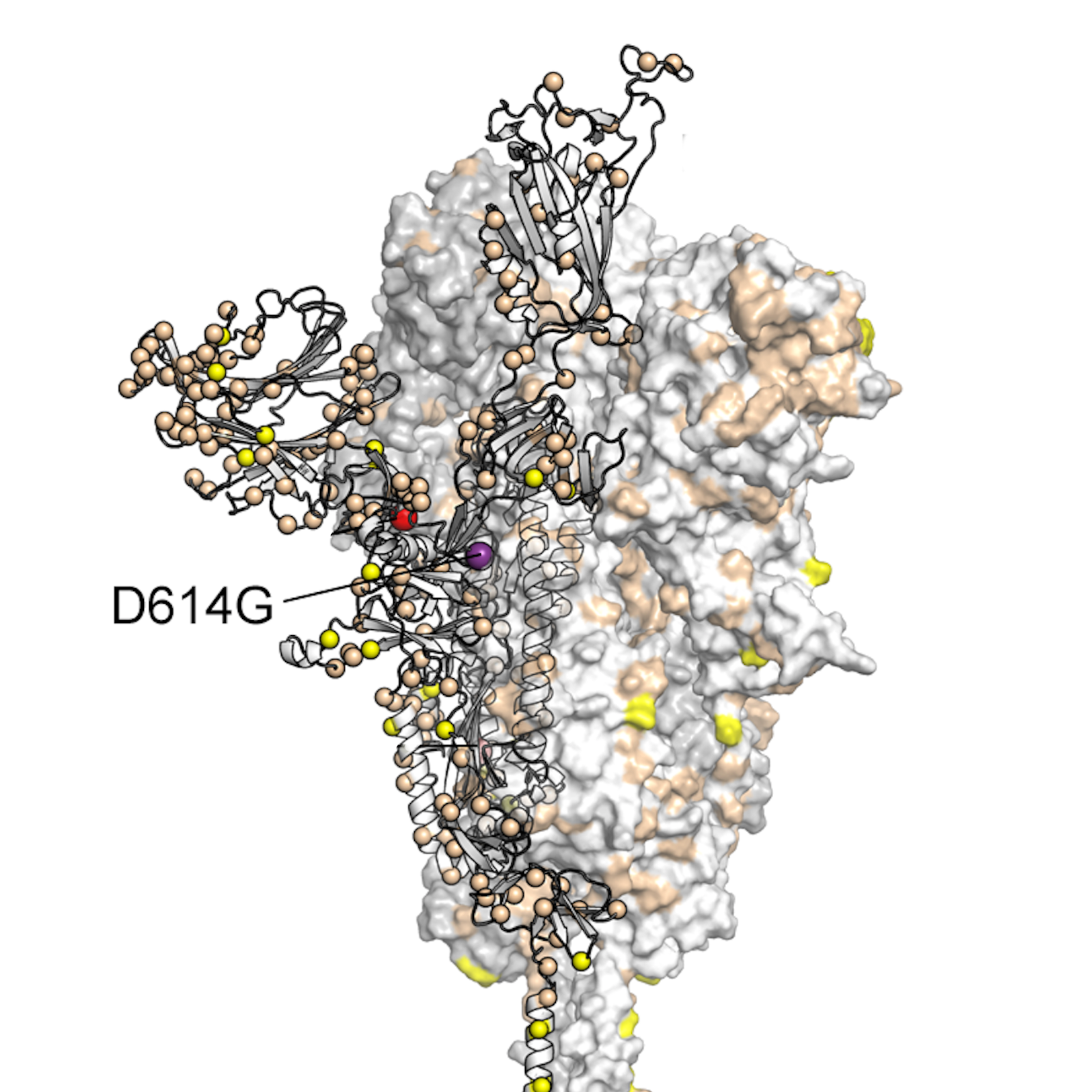
These signaling pathways include MAPK p38, ERK-1/2, and NF-κB. Several signaling pathways are thought to contribute to CD147 actions. Moreover, the concentration of CD147 is elevated in patients with inflammation and diabetes and asthmatic complications. CD147 was previously found to be the epithelial cell receptor for the measles virus. CD147 is transmembrane protein also referred to as basigin of extracellular matrix metalloproteinase inducer (EMMPRIN). clearly determined that the S protein binds to CD147 in human cardiac pericytes. Even though ACE2 appears to be the primary receptor that binds the S protein of SARS-CoV-2 to cause infection, there is evidence that CD147, neuropilin-1, dipeptidyl peptidase 4, alanyl aminopeptidase, and glutamyl aminopeptidase can act as receptors for the S protein. Several receptors have been implicated in SAR-CoV-2 infection and S protein actions in COVID-19 patients. Taken together, COVID-19 studies demonstrate that SAR-CoV-2 infection via ACE2 and the circulating S protein independent of infection can lead to cardiovascular dysfunction. It was further demonstrated that the S protein was capable of increasing cardiac pericyte migration, reduced endothelial cell network formation in Matrigel, induced pericyte cytokine secretion, and increased production of pro-apoptotic factors leading to endothelial cell death. Findings in this study determined that close to 70% of the patients did not have their pericytes infected by SARS-CoV-2. demonstrated the presence of the SARS-CoV-2 S protein in the peripheral blood of COVID-19 patients. The cytokine storm and hypoxia-induced actions leading to cardiomyocyte apoptosis is another mechanism suggested for cardiovascular mortality in COVID-19 patients. A potential mechanism for cardiac disease in COVID-19 has been myocardial involvement mediated by ACE2. The mechanisms by which COVID-19 causes or enhances cardiovascular diseases have been under intense investigation. Cardiovascular disorders such as myocardial infarction, arrhythmias, and thromboembolism appear to be a consequence of COVID-19. As such, the long-term consequences of SARS-CoV-2 on multiple organ systems needs to be evaluated. We have reached the 2-year anniversary for the COVID-19 pandemic, and it is clear that SARS-CoV-2 will become an endemic virus. Future studies are needed to determine the effect of the S protein on pericytes in other organs and evaluate the effectiveness of CD147 receptor-blocking therapies to decrease organ damage caused by the S protein. These findings support the notion that circulating SARS-CoV-2 S protein could contribute to cardiovascular disease independent of viral infection. previously determined that the S protein acting through the cluster of differentiation 147 (CD147) receptor, and another unknown mechanism had detrimental effects on human cardiac pericytes ( Clin Sci (Lond) (2021) 135 (24): 2667–2689. Experimental findings are demonstrating that the circulating S protein can bind to receptors resulting in inflammation and cell, tissue, and organ damage. Interestingly, the SARS-CoV-2 spike (S) protein can be found circulating in the blood of COVID-19 patients.
The SARS-CoV-2 virus that results in COVID-19 has been found to damage multiple organs beyond the lung.


 0 kommentar(er)
0 kommentar(er)
